Harput – Folk Medicine
Author: Adom H. Boudjikanian , 20/11/2018 (Last modified: 20/11/2018) - Translator: Simon Beugekian

Author’s preface and personal observations
From a very young age, I heard of the spiritual and intellectual contributions made to Kharpert by German, English, French, and American missionaries who had settled down in the district. I learned of the German teachers’ school and orphanage; of Pastor Ehmann; and of the Euphrates College, which was evidence of American investment in the district, and which also accepted boys and girls from other districts and provinces who were hungry to receive an education. I heard of the teaching hospitals founded by the Americans, which “produced” Armenian doctors and nurses, and which also provided treatment to the area’s Turks and Kurds. Vahé Haig’s voluminous work on Kharpert [1] was a “cornerstone” in our home. Our family’s children went as far as wondering if renowned intellectuals had been grown in the farms of our native plain [a reference to the title of Vahé Haig’s work, which translates into Kharpert and its Golden Plain].
We even knew the surnames of several “prefesors” who had taught at the Euphrates College, and who had been colleagues of my paternal grandfather’s. This grandfather of mine was called to the police station on May 1, 1915, for a “routine check,” alongside Tlgadinstsi, who served as the principal of the Central School at the time. My grandfather Hovhannes was then tortured in prison and died there [2]. His brother Boghos, a trader, as well as his sister Hripsimé, were also killed in similar circumstances. Family members told of how during those “dark days,” German and American missionaries risked their own lives to rescue Armenians by finding safe hideouts for them.

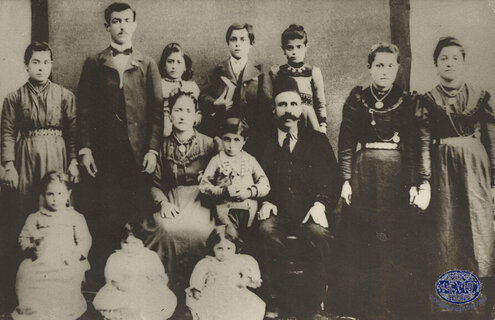
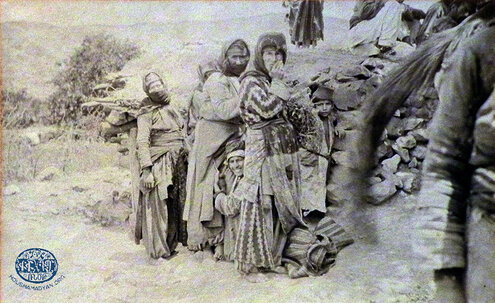
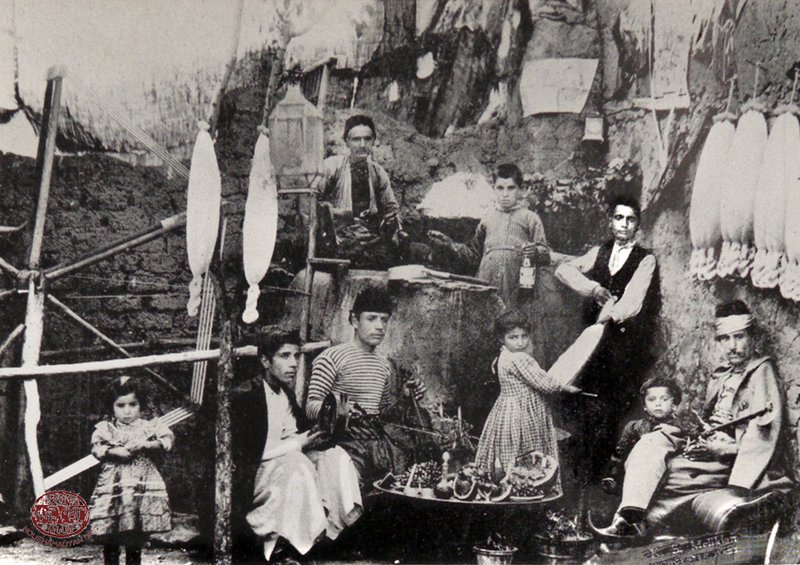
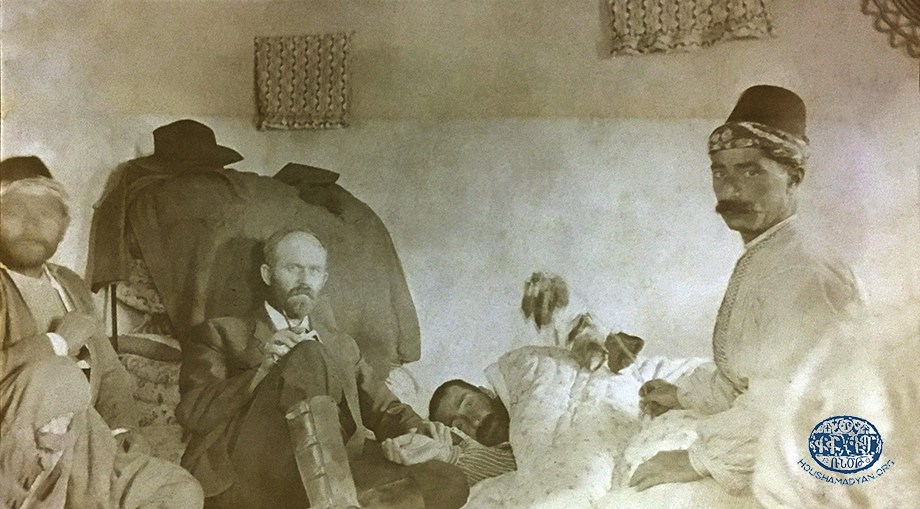
1) Harput/Kharpert. The Karadjian family, circa 1910. Standing, second from the left is Dikran Karadjian, who later married Aghavni Tashdjian. Dikran and Aghavni were the maternal grandparents of Adom Budjikanian, this article’s author. Dikran was killed in 1915. Dikran’s brother, Garabed Karadjian, holding a book in his hand, is on the right of the individual standing immediately on Dikran’s right. The others in the photograph are other members of the family, whose names are unknown (Source: Adom Boudjikanian collection, Montreal).
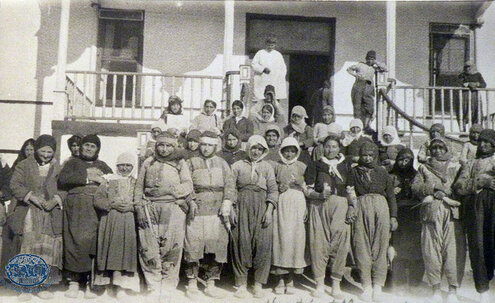
2) Harput, ca 1897. The family of Maritsa Tyufenkdjian, wife of Hovhanness Bujicanian. Left to right, standing: Maritsa’s mother Hripsime; beside her, sitting, is Maritsa’s father Karekein. Maritsa (born in 1883) is sitting in front of her father, with a white ribbon in her hair (Source: Susan Sobaje collection, Fresno CA).
My mother entrusted “Teacher” Aghavni (my maternal grandmother), the widow of her martyred father Dikran Karadjian, with our pre-primary education in the Armenian language. She taught us our miraculous language, the refrain “The people of Kharpert are always Armenian speakers” constantly on her lips. When we had toothaches, Grandma Aghavni would rub our gums with all-curing arak, while simultaneously taunting my pharmacist father – “You are prods [Protestants]. This medicine can’t cure you.” My grandmother mixed arak [for the purposes of this article, the term “arak” is used to describe potent homemade spirits] from sour cherries in her kitchen and reserved its use for special occasions. Did she “concoct” this arak only for its medicinal properties? Aghavni had worked at the Armenian orphanage in Ghazir, to the north of Beirut, managed by Swiss missionary Jakob Künzler. When I contracted urticaria (hives) after browsing through the orphanage archives that she had retained, her first reaction was – “It’s dabas, come and let me rub yogurt on it.” Aghavni always praised God with the words “love to His name.”
Kharpert was the center of gravity of our family’s social consciousness. The Kharpert Compatriotic Union was active in Beirut, bringing together Armenians native to the cities of Kharpert and Mezire, as well as surrounding villages. To this day, the Union publishes an illustrated calendar every year.
Our family’s dentist was a native of Husenig, while my father’s and my barber was a native of Kharpert. His name was Mister Yeghia (Der Manouelian), and he worked in a small booth adorned with many pictures and mirrors, located in the Rmeil neighborhood of Beirut, near the brewery. He would snip the air a couple of dozen times with his scissors before proceeding to cut my hair. He would mumble about the past, but I was too young to understand what he meant. Occasionally, he would stop his peroration and ask me in the Kharpert dialect – “Gasgnas?” [“Do you understand?”]. His son, Kristapor, would later become a renowned photographer in the United States.
The atmosphere in our home, saturated as it was with all things Kharpert, strengthened our elders’ will to survive, despite the fact that their loved ones had been martyred back in their homeland, and they had started their lives anew on “foreign soil.” Did their nostalgia perhaps engender dreams of one day returning to Kharpert?
During my late adolescence, my family’s “Kharpert-centric” mindset began seeming alien to me. Due to their parochial attitudes, they would cultivate close relationships only with their compatriots, which included the “city dwellers” and those who hailed from Mezire, Husenig, Morenig, etc. Armenians native to neighboring districts – such as Dersim, Malatia, and Dikranagerd – were also acceptable. To me, this exclusive, nativist attitude seemed incomprehensible. Was it because my family wanted to avoid those who had roots in Cilicia, and who “weren’t Armenian speakers” like we were? And what did those Cilicians think about us and others native to Kharpert? Do we Armenians practice a form of “compatriotic discrimination”?

Topography, climate, and water resources
The effects of topography, water resources, and climate on the lifestyle, customs, and primary occupations of an area, and thereby the health of the population of that area, are well-documented. Therefore, I would like to quickly detail these aspects of Kharpert’s geography.
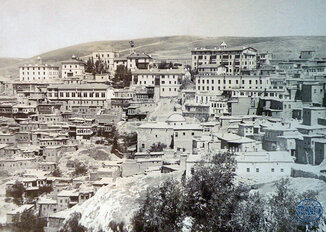
In his work Kharpert yev Anor Anmichagan Shrchanage [Kharpert and its Immediate Environs], Bedros Depoyan states the Kharpert District of the Mamuret-ul-Aziz Vilayet was a plateau ringed by the Taurus and Transcaucasian mountains. This plateau, concaving gradually, gave way to fertile fields (“the golden plain”), “adorned” by approximately 360 villages, the majority of which were Armenian-populated [3].
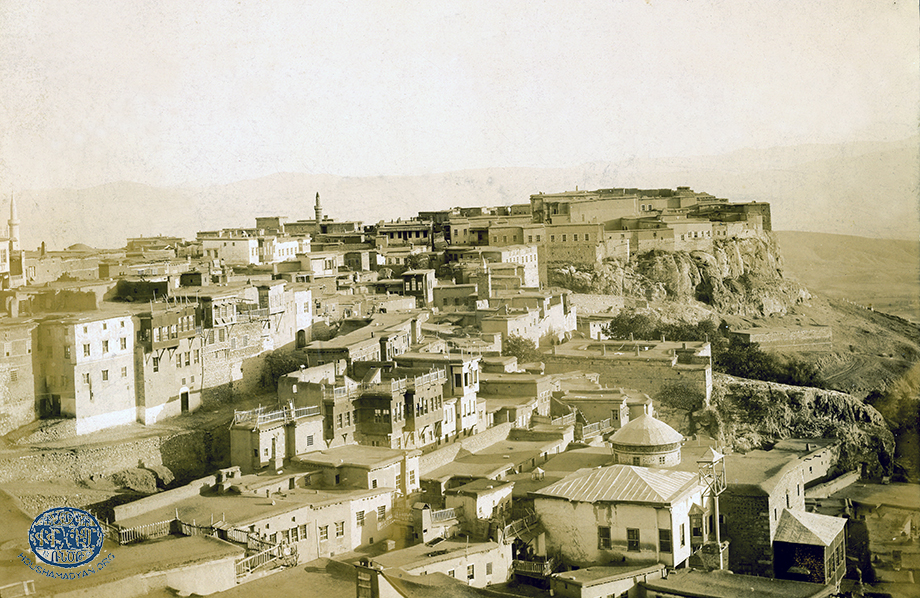
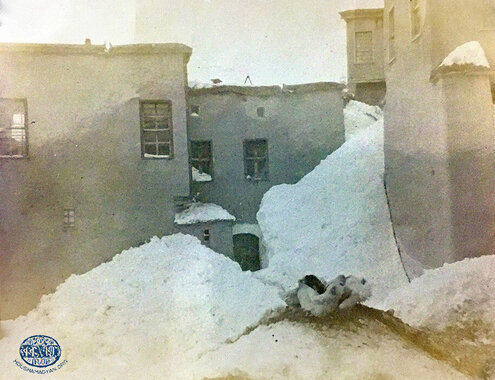
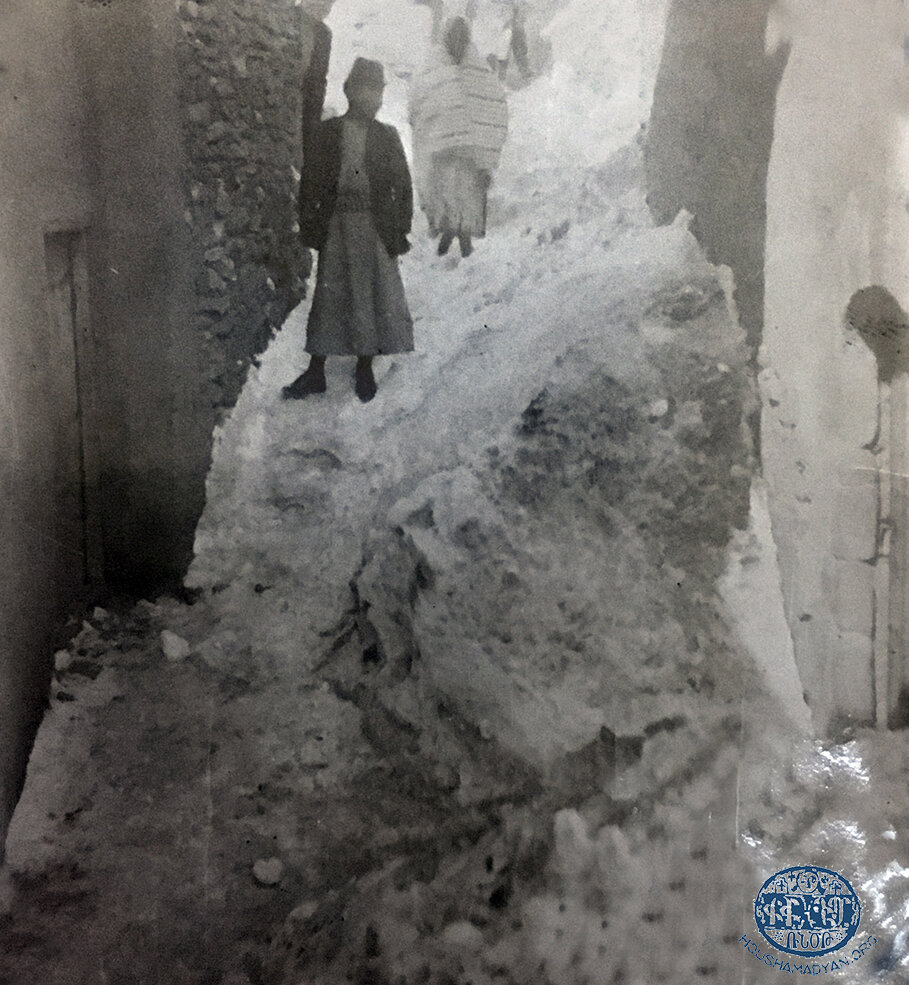
Geographic position and climate – The district was located in the east of the Ottoman Empire, almost halfway between the Black Sea in the north and Syria’s contemporary borders in the south. Kharpert’s climate was continental, with hot summers and snowy winters [4]. The residents of the city have recalled that in the winters, the snow would make the already-narrow roads of the city impassable, and the only way to move about was to do it “denre denir” [“from roof to roof”]. The two major cities of the of the Mamuret-ul-Aziz district were Kharpert in the mountains, at an altitude of 1,290 meters above sea level, and Mezire perched on a highland at an altitude of 1,074 meters, the same altitude as the district’s “golden plain” [5].

Water resources – The borders of the district consisted of the Aradzani (Murat) River in the north and the Euphrates River in the south. In effect, this meant that the area was a water-rich peninsula, which, in the summers, could lead to insalubrious conditions, becoming a swampy breeding ground for mosquitos. The local ecosystem was rich in flora and fauna. Among the cultivated crops were wheat, barley, oats, other grains, legumes, various fruits, cotton, vines, and mulberries. The Aradzani and the Euphrates were fed by many streams and runlets, the result of the spring thaws. The area’s villages had their own natural or artificial wellsprings.
Our sources indicate that the waters that flooded the fields were rich in minerals beneficial to the fertility of the soil [6]. Kharpert was home to a pond called Dzovk, which had limpid, but bitter waters. The fish known as khdoud was caught in this pond and exported, and the locals dried it and kept it as supplies for the winter [7]. Let me add here that the people of Kharpert often went to bathe in the hot waters of the Djermoug District, seeking a cure for various ailments. Alongside other mineral salts, mineral water is also rich in sulfur, and is particularly beneficial for those suffering from arthritis [8]. Given the natural mineral wealth of the area’s mountains, we may infer that Dzovk, too, had become saturated with minerals, causing the bitter taste of the water. The khdouds had probably adapted over time to the chemical composition of this water. One wonders what effect the consumption of this fish had on the health of the locals.
The people of Kharpert had developed their own unique methods of preserving food, using chunks of ice picked off the bouzloukh (freezer), located in the mountainous Sinamoud neighborhood of the city. The chunks of ice were kept in the iceboxes of each home. This bouzloukh, or to be more precise, the bouzloukhs, were piles of snow that had frozen in the deep crevices of caves, and which would not melt, even during the hottest months of the summer [9].
From this, we may be driven to infer that the people of Kharpert enjoyed relatively good health, by virtue of the clean mountain air, the presence of potable and washing water, etc. However, there were some aspects of their lifestyle that had a deleterious effect on their wellbeing. The people of Kharpert were acquainted with soap, which was imported by local merchants [10].
There was also the relatively nutritious diet the locals ate. They consumed legumes, grains, and fruits, which all grew abundantly in the “golden valley.” Though the wines produced by the vineyards were exported to the Caucasus and Russia, the wine and brandy “pulled” at home was consumed with ancestral moderation [11]. As for the cultivation of opium, it gradually gave way to the development of orchards, which put an end to the problem of opium addiction in the area, if this had existed at all [12].
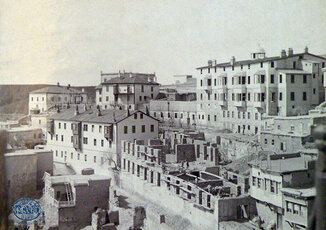
But the public health infrastructure in the area was yet to reach a high level of development. Boghos Efendi Dzeron, a belediye khalfa (city architect), mentions that in the 1870s, the villages of the Kharpert Valley, such as Parchandj, lacked basic toilets and sewer systems. “The outhouses of the homes were not provided with water. There was no modern sewage system. The cleaning of the streets was entrusted to torrential downpours, which turned the roads into impassable quagmires of mud… The outhouses often opened onto to rear courtyards of homes or onto the roads, and many were uncovered… Communal outhouses in the corners of courtyards were used particularly by the children.” It is not difficult to imagine how easily contagious diseases spread under these conditions.
In the 1870s, Boghos Efendi Dzeron succeeded in securing an official edict for his village of Parchandj, which obligated residents to observe specified cleanliness and sanitation guidelines, on pain of “fines and imprisonment.” Dzeron also introduced the smallpox vaccine into the area, and succeeded in making it compulsory for the population [13].

Crafts and industry in the Kharpert District
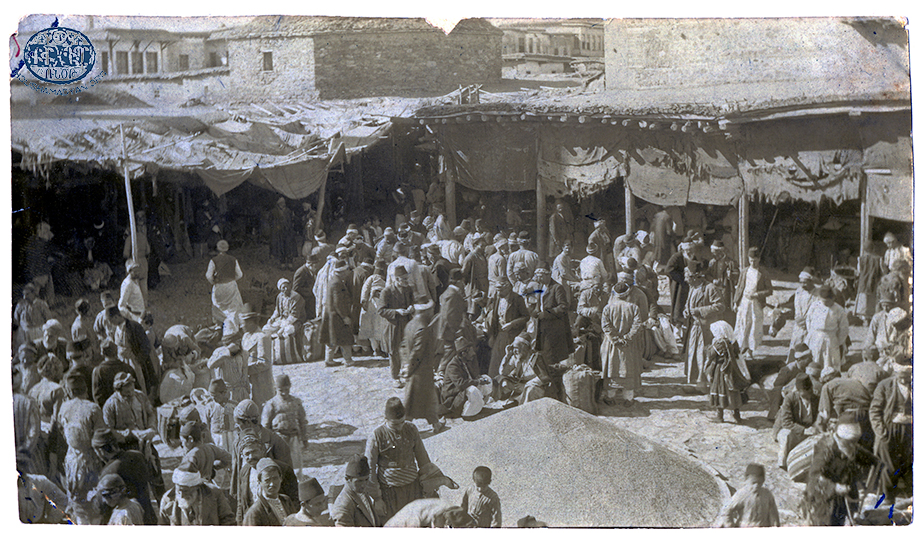
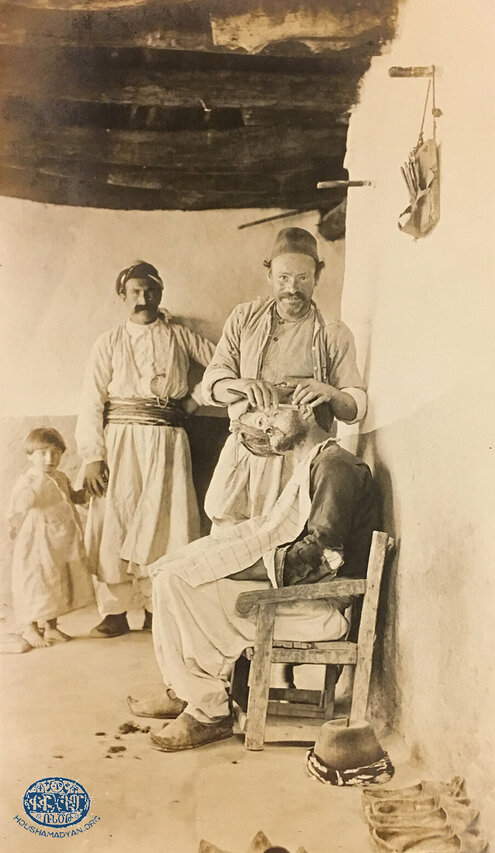
Like other Armenian districts of the Ottoman Empire, Kharpert was home to its own artisans and craftsmen. Among them, Dindjian mentions the tailors, cobblers, metalsmiths, carpenters, joiners, jewelers, butchers, clothiers, and barbers (barbers were considered to be “half-doctors” and “half-dentists”) [14].
From the public health perspective, we must underline that Kharpert was home to several large industries, mostly due to the raw materials that the area possessed. One of these industries was sericulture, itself based on the industry of the cultivation of mulberries. The larvae of silkworms were fed mulberry leaves; then their cocoons were “loosened” in warm water, producing treads of silk, which were woven together to make silk cloth. The Kharpert District was home to two large silk factories powered by steam engines – the factory of the Fabrikatorian family in Mezire [15], and that of the Kurkjian family in the City of Kharpert [16]. A large number of women were employed in these factories.
The Bakr Maden area of the district was home to a mine of copper and gold. All work at this mine was performed by hand [17]. The City of Kharpert was home to the Pariguian Brothers’ foundry, which manufactured agricultural and other tools [18]. The tanning of leather was yet another industry in the city, and several tanneries operated there. These required large amounts of water. The city’s principal tannery was located in the “lower neighborhood,” in a valley, near a large spring. Additional tanneries operated in the villages of the valley [19].
1) City of Harput. Lower neighborhood. A four-seat Ferris wheel in an amusement park adjacent to the Capuchin Church (Source: Amherst College, Archives and Special Collections, William Earl Dodge Ward Papers).
2) A barber working in the City of Harput (Source: Amherst College, Archives and Special Collections, William Earl Dodge Ward Papers).
Naturally, one cannot expect the pioneers of industry in Kharpert or Merzire to have adopted an ecological approach to industry. But we may wonder what effect the effluent from these factories, which was channeled into local waters, had on the health of the population. Carcasses of silkworks remaining in the countless discarded cocoons were toxic, as were the putrefied scraps of skin and leather discarded by the tanneries. The situation was reminiscent of Norwegian playwright Henrik Ibsen’s play En Folkefiende [Enemy of the People], which focuses on the toxic waste produced by a factory and its effect on the health of the local population.
Many cases of occupational diseases and conditions were recorded [20]. To wit, textile spinners suffered from respiratory difficulties and byssinosis, and the miners from silicosis (with symptoms including coughing, respiratory difficulties, and lung infections). Copper miners were predisposed to cancer, and those working with metals to skin conditions. How did employers attend to the health needs of their workers? Were employees dispatched to the American hospital in Kharpert to receive treatment? We were unable to answer these questions. One wonders if the likes of Boghos Dzeron sounded the alarm on the effects of industry and crafts on public health.

Treatments related to the beliefs of the people of Kharpert
Like their compatriots in other districts, the people of Kharpert often had recourse to superstitious means of medical “treatments.” They resorted to these practices to ward off evil spirits – which, in their terror, they always called “our betters” – or alks (enemies of the sons of Adam). They often sought supernatural medical intervention by performing pilgrimages, appealing to supernatural forces or benign spirits, and sought to avoid the actions of evil spirits. Information regarding these beliefs could be obtained for the villages of Parchandj and Tadem, and it is likely that they were held more generally by the people of the other villages in the valley.

Superstitions, supernatural beings, and protection against them
Spirits – According to local beliefs, spirits like the djins were not inherently evil, but would become “enemies of the sons of Adam” if their names were uttered openly, or if rocks were tossed into the wells they inhabited alongside their families. One had to beware of angering these spirits, for they would become “a plague and a blight upon the home” [21]. Spirits who were inherently evil were called alks.
Shvods (female ghosts) – They attacked newborn children and pregnant women.
The evil eye – Winsome children, as well as productive milk cows and prized buffaloes were protected from the evil eye by talismans tied to their hair or fur. The sick hung silver, triangular amulets that contained magical incantations from their necks [22].
Apsons (incantations) – These were passages from the Bible and special prayers, each reserved for a specific situation. Here, we present two examples. The first was used to heal wounds, and was known by the name of yeres krel: “Pazoumvoghorm Der… Kahanayagan aghotuk zhivants pjshgel… Srpya zaghdeghoutyun yeresats yev ampoghch marmno sora…” [“All-merciful Lord… I beseech you with this priestly prayer to cure the sick… Wipe this filth from my face and body…”]. A second incantation was probably used to bring an end to shakes/convulsions brought about by malaria – “Der Asdvadz mer… Esd Asdvadzayin hramanit, gabemk ztoghs… Togh ztoghs i dzaraye koumme… Ayjm yev mishd…” [“Dear Lord… with your Godly order, put an end to my shakes… May they serve your will… Now and forever…” [23].

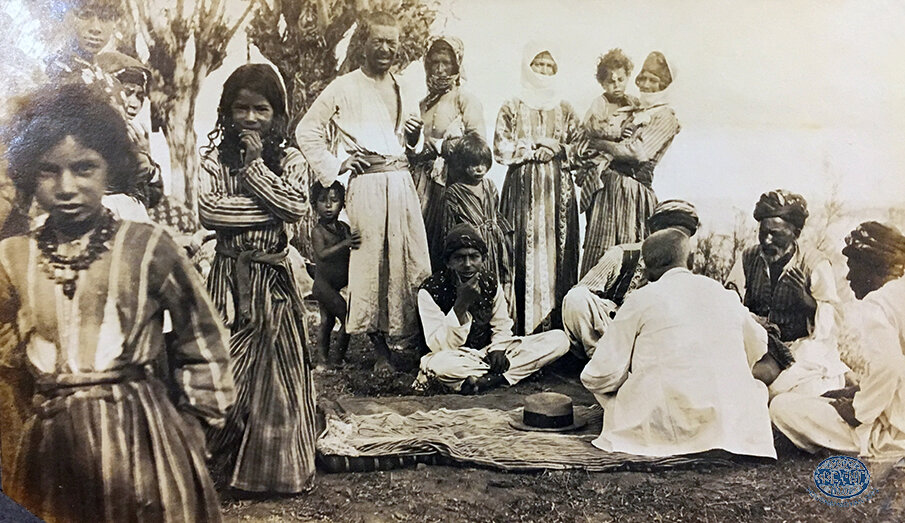
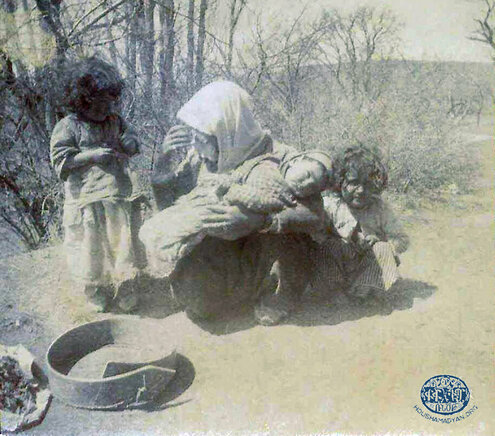
1) A mother and her children in Harput (Source: Rigsarkivet/Danish National Archives, Copenhagen. Courtesy of Matthias Bjørnlund).
2) A Kurd from the Harput area with his horse. Standing to his right is probably his daughter (Source: Amherst College, Archives and Special Collections, William Earl Dodge Ward Papers).

The immediate care of newborns and mothers in labor, and superstitions regarding their health
Shvods were female spirits (djins), also known as Adamorto doushman (enemies of the sons of Adam, or more generally enemies of men). In Parchandj, to protect a woman in labor from these spirits, an iron cross and hook were placed on her right side. Otherwise, the shvods would come and rip out her liver with their own hooks, take the newborn infant, and substitute him or her with a deformed child. To ensure their newborns’ continued protection, parents in Kharpert had a priest read protective prayers and shake his chasuble over their children for 40 days after birth [24].
Like the people of Parchandj, the residents of Tadem protected mothers in labor from evil spirits by keeping the hook used in their tonirs under the birthing mothers’ pillows. An ugly child was labelled an alkoupokhadz (substituted by alks). To protect against djins, the newborn’s and new mother’s bed were ringed with ropes of hair. Childbirth was supervised by the experienced village midwives, who would remain beside the new mother’s bed for days after birth, protecting her from alks [25].
Tabgha – It was absolutely taboo for pregnant women to receive visits from certain individuals. It was believed that the presence of these individuals would bring catastrophe upon the growing fetus or the newborn – meaning miscarriages or stillbirths. Moreover, such a “curse” had the potential of being passed down from one generation to the next. Two of these tabgha visits were the following: a pregnant woman could not visit another woman who had just given birth within the first 40 days of the latter’s labor; and newly wedded couples had to refrain from visiting other newly wedded couples within the first 40 days of their marriage. If these rules were broken by accident or due to understandable circumstances, there was still one way to avoid the curse – the women would trade sewing needles, and the men would trade two coins. If the individuals involved also neglected to conduct this ritual, the only way to break the tabgha was for the women to jump over a newborn cat or dog while crossing themselves and chanting “tabghas tser vra tapi” [“May my tabgha fall onto you”] [26].

The first of the aforementioned proscriptions can be explained scientifically. Women sometimes contracted post-partum infections after childbirth due to unhygienic conditions during childbirth or the contamination of implements used during it (dirty hands, household items, towels, etc.). The first to draw attention to the danger of lack of proper hygiene during childbirth was Hungarian doctor Ignaz Semmelweis (1818-1865). To prevent infections, he introduced sterilization protocols in birthing rooms [27]. Prohibiting new mothers from visiting other pregnant women so soon after birth, while their own health status (whether they carried infections or not) was still unknown, prevented infection to the fetus or newborn infant.
To give the readers an idea of the “refined” methods used by midwives of Parchandj, we can cite the example of popular midwives Makho and Merar Mro bajis and their peers: when a woman in labor had difficulty passing the “infant’s friend,” meaning the placenta, they would have the mother “mount” the handle of a shovel (or would they insert the handle into the vaginal passage – our source is not clear) and would rock her up and down until the placenta was released. As a result, mothers were at risk of contracting abdominal infections, which could be fatal, or would condemn them to a lifetime of pain. It is easy to imagine the types of bacterial infections that could result from such primitive “obstetric” practices. As for the placenta, the locals would bury it in a safe corner, so that pets did not eat it. Alongside the placenta, they would also bury the scissors used to sever the umbilical cord, so that it wasn’t ever used for anything else. Otherwise, according to Makho Baji, the child would die [28].
Newborns were immediately rubbed with salt and left unwashed for a whole day, to ensure that their “bodies grew to be mature.” Then, they would be bathed with hot water, hung upside down to ensure that they had “tall figures,” and held by the head so that they would have “long necks.”
The parents sprinkled the newborn’s first clothes with ashes of “chagha soil” to protect against heat rashes. They would cross the infant’s arms three times on the chest, according to Christian tradition, then swaddle them tightly, almost as tight as mummies. It is doubtful that the crossing of the chest three times protected the newborns from salt burns and from the salt being absorbed into their skin. The salt could potentially make its way through the skin and into the bloodstream, disturbing their bodies’ natural mineral balance and causing poisoning. This custom of “salting” newborns is also documented in a region quite far from Kharpert, in Gesaria (Kayseri), which presumably indicates that the custom was also practiced in other villages of the Kharpert Valley. In Gesaria, only children’s armpits were rubbed with salt, which went some way in mitigating the extent of poisoning [29].

Holy sites and bodies of water endowed with healing powers
These were churches, monasteries, trees, or bodies of water that possessed miraculous healing powers.
-The frankincense tree of the Morenig Village: The village was home to the Saint Sarkis Church, and beside it, a large frankincense tree. Seeking cures for their diseases, people would tie variegated strips of cloth to the tree’s branches, and would toss old or new coins into a hollow in the tree’s trunk. According to E. Sirvart, many returned home cured. During the 1895 Hamidian massacres, a Turkish woman from the village stole money from the tree’s “safe.” As a result, she fell ill and “her mouth became crooked.” According to legend, a bearded man then appeared in the woman’s dreams on three separate occasions, advising her to return the money to the tree. Finally, she decided to act on the advice. Upon returning the money to the tree, she was immediately cured, and she even made an additional donation [30].
The status of the tree as a sacred object was probably related to the resin it produced, which was processed into an aromatic incense containing essential oils with certain therapeutic properties [31]. Additionally, the mysticism associated with the incense permeating churches could have resulted in believers experiencing the placebo effect, whereby, theoretically, individuals may perceive a certain result based on the strength of their expectations.
- The Holy Virgin: This was an Assyrian church located in the City of Kharpert. Turks and Kurds, too, visited the site in the hope of cures for their ailments. The site was celebrated for healing all forms of conditions. The handicapped, the blind, lepers, the possessed, and others suffering from mental illnesses all made pilgrimages to the Holy Virgin. Visiting pilgrims lodged in furnished rooms provided by the church [32].
- The Saint Areon (Saint Aaron) Rock: It was located on a rocky escarpment near the bouzloukh in the Sinamoud neighborhood of the City of Kharpert. This holy site was celebrated for preventing the deaths of newborns and infants, which was an exceedingly common occurrence in the area. On every Saturday on the eve of Ascension Day, pilgrims, carrying their children, would converge on the rock on horseback, on donkeys, and sometimes even in bare feet [33].
- Naderbaba: This was a small hut, with windows, built atop a rock in the upper neighborhood of the City of Kharpert. The site had once been the grave of a Turkish soldier. It, too, was a pilgrimage destination for Armenian and Muslim mothers trying to protect their newborns and infants from death. They would sprinkle handfuls of dirt from the grave onto their children’s heads, hoping that their pilgrimages would be rewarded [34].

The holy sites/healing sites of Husenig
The people of Husenig put great store in their saints and shaped their lives and beliefs according to their wishes. In exchange for their piety and fervor, they expected miracles, including miraculous cures [35].
Here are some examples of Husenig’s “healing” sites –
- Saint Varvara (Saint Barbara) Church: This church was dedicated to the memory of the daughter of a wealthy man from Kharpert. Legend held that during pagan times, the daughter had been killed by her father for converting to Christianity. Pilgrims visited the church seeking cures for eye disease, as well as for infants who could not speak [36].
- The Kouk-kou-lou-lou (Gougouligou) Holy Site: Varvara’s father, Serid Kasem, had also ordered the execution of Varvara’s maid, who had accepted the Christian faith alongside her mistress. In her death throes, the maid’s final gasps sounded like a crowing rooster. This holy site was visited by the deaf seeking a cure for their condition [37].
- The Saint Mariané (or Saint Maran) Rock: According to legend, Marian was a saint from the City of Alexandria whose fame had spread all the way to Kharpert. She appeared in the dream of one of Husenig’s residents, perched atop a rock in the valley outside the city. Thereafter, that location was designated as a holy site. Armenian mothers visited the site, seeking the saint’s blessing upon their children who had not begun to walk yet [38].

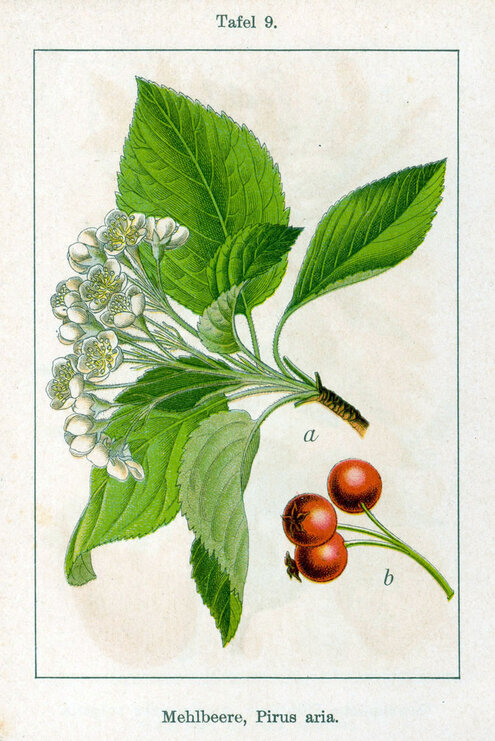
Miraculous Waters
- The spring/pond under the whitebeam tree in the Village of Keserig: The whitebeam (Pyrus or Sorbus aria) was a tall, wide tree that produced small, yellowish fruits. Those seeking treatment would bathe in the pool under this tree. If they tied a ribbon from their clothing to the branches of the tree (as a symbol of the sickness that was left behind), they were certain to be cured. If a faithless Christian approached the tree, the ribbons would rain down upon him or her [39].
- The spring/pool near the Saint Mergerios Monastery in the Village of Ichme: Pilgrims would spend the nights in the monastery compound or in tents pitched near it, in the hope that the saint’s intervention with God would result in miraculous cures for their conditions. For this to happen, the pilgrims had to first drink from the spring and bathe in the pool [40].

More objective forms of popular medical treatments
Among these methods were water therapy, which was used in cases of arthritis (hot springs and mineral waters); naturally-occurring medicinal treatments (herbs, animals, and minerals); surgical treatments; osteopathy; and bone setting/orthopedics.
Treatments for infertility
In an interview, Khatoun Mouradian, a native of the City of Palu near Kharpert, revealed two phytotherapeutic and osteopathic methods to treat infertility [41].
- Medication consumed internally (first part): a paste was prepared using unwashed sheep’s wool and pig’s lard. Then, ground buds of cloves were mixed with ginger root and chickpeas. This mixture was kneaded into the paste of wool and lard, and the resulting product was given the shape of an egg. The wool served as a “receptacle,” from which the oil-soluble active pharmaceutical ingredients of the mixture would gradually be absorbed by the body. To the final, egg-shaped “pessaries” were affixed unwashed “tails” of blue thread, using a glutinous plant-based sap.
These devices were inserted into the uterus and kept there for 24 hours. This process was repeated seven times. Then, a midwife would lay the infertile woman down in the prone position and massage the skin on her back, while holding her ankles against her back. The midwife would hold the patient in that position and rock her, in order to induce the uterus to “sit back in its place.”
- Medication administered externally (second part): Ground buds of cloves, ginger, and incense were mixed with black tar and made into a paste. This paste was then spread on two unwashed rags. These rags were heated over fire and separately applied to the infertile woman’s back and lower abdomen. A separate paste would be prepared, using sheep’s wool and soft lard. A boiled egg would be covered in this paste, and a string would be tied to it. The egg would then be inserted into the subject’s uterus, where it would be left for a certain period of time. The subject was advised to engage in sexual relations upon the removal of the egg.
- Adoption: If these treatments failed, families in Kharpert resorted to adoption. According to Hripsimé Nakkashian-Ghougasian, a native of Kharpert, an adoptive mother would slide the adopted child down the neck of her dress, all the way down to the hems, thus simulating the act of giving birth. Moreover, in cases of infertility, husbands were forbidden from seeking divorces from their wives.
- Female infertility has many causes. Without going into details, some of these causes include hormonal issues; infections or inflammation of the uterus, ovaries, or the fallopian tubes; disorders that interfere with the production of eggs or regular menstrual cycles; etc. [42].
The midwives of Kharpert were probably ignorant of these medical facts. However, we must recognize that they knew of the uterus’s existence and the role it played in childbirth. They may not have known of the existence of the ovaries, but they knew that new life grew out of an “egg,” and for that reason, they molded their “pessaries” into the shape of eggs.
As for the compounding of these remedies, it is astonishing to us, in present times, that the midwives of Kharpert made use of such advanced intrauterine devices (IUDs). These interventions featured a non-soluble core/receptacle (the sheep’s wool) surrounded by a layer of potent fat-soluble herbal components. This cocktail of herbs was considered to be a panacea for all cases of infertility. Scientifically speaking, cloves have antiseptic, analgesic, antispasmodic [43], and antibiotic [44] properties, and also stimulate the nerves. Ginger has the same properties as cloves, and stimulates the circulatory system [45]. Another important point – according to an expert source, ginger may stop spams of the uterus muscles [46]. Continual contractions of the uterus can impair the process of nidation, causing embryos to be expelled and preventing pregnancy [47]. The midwives’ massages probably readjusted certain sexual organs and opened passages that had been blocked.
Care of newborns
- Midwives would rub some of the blood from the newly severed umbilical cord onto the newborns’ faces, so that they would have red cheeks. This blood had to remain smeared on the face until the newborn’s first bath [48].
- Nursing of newborns: Nvart Sirounian-Sarkisian, a native of Kghi, a city near Kharpert, worked for a several years, beginning in 1919, in the American orphanage of Kharpert. She stated that if the mother was lactating and the newborn’s suckling instinct had not yet developed, the mother would nurse a dog pup to relieve the pressure in her breasts [49]. Different methods were used to limit the amount of lactation and in weaning a newborn off breastmilk. For example, to gradually stop lactation, compresses of cold rags were applied to the breast to slow down the lactation process. Or, again according to Mrs. Nvart, pickled leaves of cabbage were wrapped in towels, and the breasts were covered with these towels. According to modern phytotherapy, cabbage (Brassica oleracea), alongside other uses, may be used to relieve and empty engorged breasts. Experts have experimented with ways to place cabbage leaves in brassieres or to use ointments made of cabbage [50].
- Nvart Sirounian-Sarkisian, and Varter Zakarian from Harsig, a village near Kharpert, both stated that women were not allowed to nurse if they became pregnant very soon after childbirth. Under such circumstances, it was believed that lactation could harm the fetus [51]. There is some scientific support for this belief. According to the American Pregnancy Association, when an infant suckles on the nipple, the mother’s body produces a hormone called oxytocin, which can cause small contractions of the uterus. Although it is believed that these contractions are not intense enough to cause a miscarriage, there are cases where the mother’s health status compels doctors to advise her to cease nursing [52]. It would be interesting to know how the midwives of Kharpert had reached their conclusions. Had they observed instances of miscarriages that had prompted them to include the proscription of nursing by pregnant women in their unwritten medical rulebook?
Skin conditions
- Mrchnpon: This was the name given to clumps of small bumps on the skin, which caused excessive itching. The condition was reminiscent of a nest of ants and its surrounding area [in Armenian, mrchnpon is a portmanteau of “ant” and “nest”]. One version of the condition mostly affected the skin of the elbows. In the 1960s in Beirut, a doctor from Kharpert treated this condition with Calamine lotion™. According to Mrs. Tertsagian, who received this information from her paternal aunt, reporting the recipe of her grandfather who was a native of Kharpert, the people of Kharpert treated mrchnpon with ink [53]. At the time, ink was made of a solution of certain salts of metals and oak gall, which is rich in tannins. Both are astringent substances and have antiseptic qualities, and therefore, they could have effectively treated itching. Tertsagian adds that the treatment, which was accompanied by the chanting of an incantation (the appropriate prayer to cure oneself of this condition), had to be performed within three nights of a new moon. Her grandfather had lived in Dersim for two years, and there he had studied to become a hekim [doctor]. Dersim was another Ottoman district adjacent to Kharpert.

- Daroug (chiban of Aleppo or Aleppo boil) [54]: This condition was also known as “Bouton d’Alep” or “Bouton d’Orient” in French [oriental sore]. The condition resulted in deep lesions all over the bodies of adults and children, and was caused by the bite of the female phlebotomine sandfly. The insect’s bite introduces a protozoan organism of the Leishmania variety into the victim’s organism. The condition is scientifically known as cutaneous leishmania [55]. The sandflies that spread the disease were endemic to the riverbanks of Syria and Iraq. They made their way from Aleppo to waterlogged Kharpert, and on to Dersim.
The people of Kharpert treated them with a paste consisting of chicken manure, a puree of ground wheat (rich with starch), and grime collected from teeth. We can make some assumptions about the curative properties of this mixture. According to Wade McCall, chicken manure is rich in several chemical elements, including potassium, phosphorus, copper, iron, magnesium, and sulfur [56]. The beneficial effects of sulfur on skin conditions is well-known. Meanwhile, human saliva (which would be present in the grime of teeth) contains proteic derivates, such as histidine-class polypeptides, which have antifungal and antibacterial properties. Another protein contained in saliva, lysozyme, plays a role in the human body’s immune system. As for α-amylase, it is an enzyme present in the saliva, it converts the starch hidden in gaps between teeth, into sugar [57]. We know that the sugar produced by this enzyme, when applied to the skin, has healing properties. But our ancestors had not relied on pharmaceutical knowledge when inventing this very “appetizing” concoction.
- Another treatment for daroug, practiced in the Village of Habous: This village’s “wise grandmothers” would collect herbs from the fields, grind them, then mix the result with sheep’s bone marrow. The resulting paste was applied to the sores. Unfortunately, our source does not specify the herbs used for the mixture. Modern science is well-aware of the beneficial properties of several components of bone marrow, particularly on the function of leucocytes and the lymphatic system. These components can also neutralize alien or toxic substances within the body. Upon the administration of this treatment, the boils would “disappear and heal within a few days” [58].
- Various skin lesions and wounds: In Kharpert and Dersim, locals would boil “newborn mouse pups in oil” and apply the resulting infusion to the affected areas. To prepare this mixture, live mouse pups would be drowned in a bottle of olive oil and would be left in it for two months [59]. The solution would probably contain tissue from the pups’ carcasses that had antibacterial and healing properties. This treatment was used in Habous, where “deep cuts reaching the bone were treated using this infusion.” Mrs. Tertsagian, too, mentions the use of this treatment. She had heard of it in Aleppo, from the wife of his father’s uncle, who was a native of Kharpert [60].
- Sigil/Sinir (warts) and kordnpshdig: The former resulted in small, spongy warts on the hands, elbows, and the soles of the feet. These would bleed and cause pain if rubbed vigorously. The latter (kordnpshdig [“toad warts”]) resulted in a large number of painless warts growing on the hands. According to popular belief, these were the result of the affected area of the body being exposed to toad’s urine. The common treatment for kordnpshdig was to toss pebbles from a home’s roof on the night of a new moon, so that the boils would disappear like the pebbles. This act would be accompanied by the recital of the appropriate incantations (prayers). As for sigil, the locals would tie a silk thread around a new wart, and it would drop off within a few days [61].
We can explain the treatment of sigil scientifically. These excrescences are the result of viral infections. Research conducted by Singh demonstrates that the silkworm, its cocoons, and silk threads contain substances that have antibacterial and antiviral properties [62].
This method of treating sigil once again demonstrates that the empirical nature of many “simpleminded” rustic treatments used by the people of Kharpert have been vindicated by modern science.
Treatments of various types of pain
Unsurprisingly, in a district with advanced craftsmanship and industry like Kharpert, respiratory, throat-related, and other health issues were prevalent, as a result most people’s working conditions. Many of the popular occupations in Kharpert, including sericulture, furriery, and metallurgy, involved work in insalubrious environments and conditions.
- Eye Pain: Those who suffered from pain in their eyes (mostly adolescents and youth) were often bed-bound for weeks at a time. Their eyes swelled shut and became infected. Without early action to treat the condition, the patients would be condemned to blindness [63].
Treatments for eye pain – the milk of a woman nursing a female infant was dripped into the affected eyes. Most probably, the natural oils in the milk dissolved the sticky puss that kept the lids shut, while the immunoglobins fought the bacterial infections. According to Shahbazian, in particularly difficult cases, a cloth doused in urine or “red medication” would be pressed onto the affected eye. “Red medication” was the local name for mercurochrome solution, prepared by in pharmacies. The precursor of mercurochrome had been discovered in 1889 by Dr. Dunning, in the United States. Later, thanks to slight chemical adjustments, this substance also gained antiseptic qualities [64]. The same source states that mercurochrome is used to treat eye injuries.
Shahbazian does not mention who exactly prepared mercurochrome solutions in Kharpert. But he also mentions a pharmacy called Euphrates, which was opened in 1901 by Pilibos Movsesian, a graduate of the American University of Beirut. This pharmacist prepared and supplied medications not only to the people of Kharpert and Mezire, but also those of distant areas, like Pertag, Agn, Arapgir, and Diyarbakir. Movsesian and the pharmacists who followed in his footsteps also collaborated with missionaries like Dr. Usher and Dr. Atkinson [65]. Based on these facts, we can reasonably conclude that mercurochrome solution was prepared by the Euphrates Pharmacy.
- Abdominal pains: The abdomen houses many vital organs, like the stomach, the intestines, the liver, the kidneys, etc. Whenever one of these organs was stricken by disease, the people of Kharpert simply complained of abdominal pains, the “panacea for which was arak,” according to Shahbazian. However, we do not know exactly how arak was used – was it consumed internally, or was the abdomen rubbed with it? To this day, alcohol is used as a local anesthetic. We also know that alcohol consumed internally acts on the central nervous system as an analgesic. This is evidenced by a study conducted by Trevor Thompson, featuring 404 participants. The study’s conclusions support the popular belief that alcohol is an effective anesthetic [66]. But what did the people of Kharpert do if alcohol were not enough? They would cover the abdomen with heated clay lids, and they would also resort to massaging the affected area. These interventions could be effective in some cases, but subjects who suffered from stomach ulcers or diseases of the cecum were often doomed to die [67].
- Back pain (khoulindj): The condition pas particularly prevalent among the elderly. The cause of most back pain must have been vertebral subluxation, well-understood by modern science, which occurs when intervertebral discs erode due to old age or due to lifestyle (unnatural posture or movements for an extended period of time). The nerves are then impinged upon, causing pain. Shahbazian mentions the following method for spinal corrections: a plank of wood was stretched across the shoulders. The subject held this plank with both hands very tightly, and then pushed backwards with his or her back against the plank. This would cause the audible cracking of bones, which meant that the “khoulindj was broken,” and the patient could be sure of recovering. In cases of extreme pain, it was imperative to perform cupping therapy [68]. Notably, the aforementioned treatment involving the plank of wood is reminiscent of modern chiropractic practices.
- Toothache: In cases of mild toothaches, the locals used salt water, arak, or other painkilling liquids. Loose teeth were extracted by barbers [69].

Communicable diseases
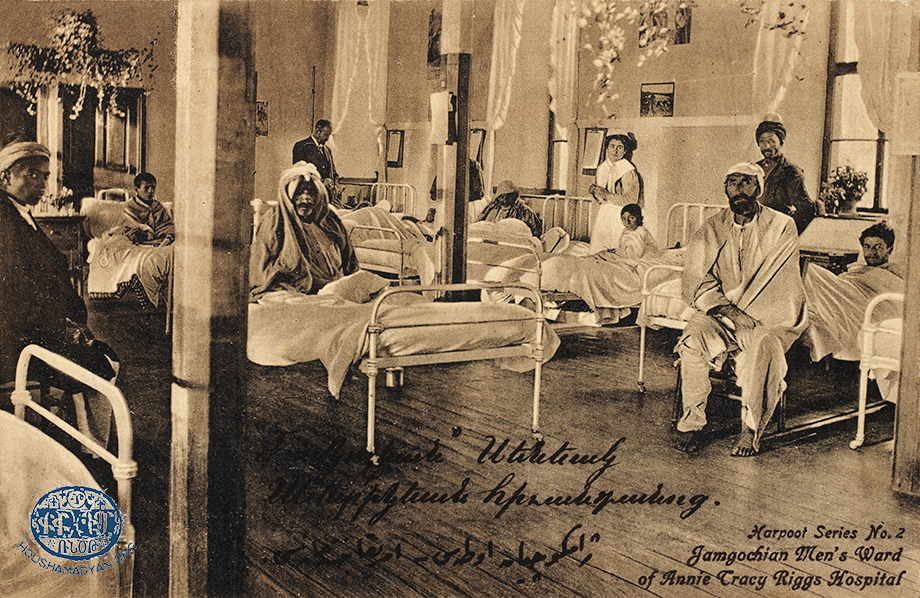
According to Djizmedjian, Kharpert was awash with communicable diseases, “despite the purity of the air and water.” He adds that “the people’s ignorance and the lack of medical care” resulted in a large number of fatalities among children and youth [70]. This assessment of the district, which was always proud of its educational institutions and intellectuals, seems baffling at the very least. Especially as the Euphrates College had established a program in obstetrics, taught by expert teachers [71]. Moreover, in 1909-1910, Mezire became home to the Annie Tracy Riggs Memorial Hospital [72]. But as we have seen, industry and crafts in Kharpert were relatively advanced, and resulted in the pollution of the local air and water. Additionally, the promiscuity that spread among factory workers, and the custom of large families living together, contributed to the spread of disease. There were also other factors that contributed to contagion, such as the area’s primitive sewage system and the slow rate of the spread of health information among the local population, despite the best efforts of Boghos Dzeron and others like him.

Communicable diseases among children
- Smallpox and scarlet fever: Djizmedjian mentions several disease, for which vaccines became compulsory thanks to the efforts of Boghos Dzeron. Among these were smallpox. Djizmedjian also mentions epidemics of measles and scarlet fever, which caused widespread fatalities, particularly among children. Sometimes, up to three children of the same family would die in these epidemics [73].
Our sources do not mention any treatments for measles. As for scarlet fever, Djizmedjian makes particular mention of the countless calcium sulphite tablets prepared by the Euphrates Pharmacy, and which were distributed at no cost to treat or prevent the spread of the disease [74]. This disease is caused by a bacterium of the staphylococcus type, and symptoms include throat pain/coughing, characteristic bumps on the tongue, redness of the face and the body, and high fever [75]. Given that scarlet fever may spread via infected droplets present in coughs, the disinfection of the throat is an important part of the treatment regimen. In the absence of modern antibiotics, the Euphrates Pharmacy distributed calcium sulphite tablets, which have antibiotic properties.
However, according to Dindjian, in the Village of Khokh of the district, the treatment of smallpox and scarlet fever was identical to the treatment of “the shakes” (see the section below on malaria), and was administered by elderly women who knew how to prepare the required herbal remedies [76]. While it is true that many herbs have antibacterial properties, Dindjian does not specify which herbs were used or how. Herbs and plans that were used heavily in folk medicine and are known to have antibacterial properties include the rind of cinnamon roots (Cinnamomum zeylanicum), dried clove buds (Syzygium aromaticum), and garlic (Alliumsativum) [77].
- Malaria (shakes): This disease can spread from person to person only in cases of blood transfusions. Malaria was also known as togh [shakes], a name evoking the convulsions symptomatic of the disease. The peak of malaria season in Kharpert was the month of August [78]. The area was waterlogged, and its waterways probably turned to swamps during this hot and humid month, allowing anopheles mosquitoes, the main vector of the spread of malaria, to multiply. When these mosquitoes bit people, they infected them with a unicellular parasite known as plasmodium, which attacks the red blood cells. Plasmodium completes a full life cycle inside the body of the infected host, and during that time the stricken individual endures different crises in different phases of the disease, including elevated fever, pain in the head and the body, excessive sweating, delusions, and the characteristic intense convulsions [79].
The shakes/convulsions are the body’s response to the fever, but when they occur for extended periods of time, the continual trauma can cause lesions in the tendons, resulting in pain. Shahbazian writes that in Tadem, there was a spring called Medzn Aghpur (Big Spring), where patients suffering from shakes were taken for treatment. They would douse their bodies with the waters of the spring seven times, while an elderly healer recited the appropriate prayer over them. As they left, they would leave a fresh egg in the spring’s pond. According to Shahbazian, the patients would be healed within two days of performing this ritual. A cold bath relaxes the tense muscles, counteracts fever, and stimulates lymphatic circulation, strengthening the patient’s immune system. But the role of the egg is more difficult to ascertain…
- Jaundice: This disease is characterized by the yellow/dark appearance of patients’ skin and the whites of their eyes, as well as the discoloration of stool. Shahbazian writes that the victims of jaundice were mostly youth, who became weak and lost their appetite. The treatment was as follows: the patient would drink the urine of four- or five-year old children every morning for three days, on an empty stomach. If this did not have the desired result, the local barber would cut the inside of the patient’s lip, thus ensuring a full recovery [80].
Jaundice occurs when for any of several reasons, bilirubin (a substance that is naturally present in the body, and a byproduct of old blood cells) remains in the blood stream (hyperbilirubinemia), instead of making its way to the gall bladder, and being excreted through the intestines. Several conditions may cause this to happen, including kidney stones, pancreatitis, infection by the Epstein-Barr virus, and hepatitis A, B, or C. Hepatitis B and C are viral infections, and are also contagious [81]. We have already mentioned that drinking urine was considered to be a treatment for jaundice. We know that urine has some antiviral properties, thanks to the presence of ammonium salts [82].
“Vay leghis prtav!” [“My gallbladder has ruptured!”] is a common expression in Armenian, used when one experiences terror. The result, according to popular belief, would be the “catching of jaundice.” In Kharpert, the only way to prevent this result was to “trap the fear.” According to S. Tertsagian, whose information comes from an informed family member, the affected individual would abstain from breakfast for three days. Every morning, the healer would lay the patient down in the supine position and apply strong pressure on the two inguinal ligaments (at the top of the thighs, where they connect with the torso). This sudden application of pressure could stimulate the gallbladders to start working again. Another method of treatment was to douse the patient with cold water, so that the gallbladder, blocked due to fear, relaxed and began functioning again. A third treatment was to burn the patient with burning tobacco [83].

- Tuberculosis: Shahbazian writes that this deadly disease was rare in the villages of Kharpert. When it occurred, it was attributed to “the insurmountable yearning caused by love.” To treat the disease, the locals would induce nausea in the patient, until the latter began vomiting and expelled the disease. For example, they would tell the patient that he or she had just eaten dog meat [84].
- Khlrtoug: This disease was thought to be caused by infections originating from the urine or feces of female moles (khlourt in Armenian). A swelling would appear somewhere on the patient’s body, and this protrusion would “travel” across the body before bursting and become a large blister. As a treatment, the patient would be fed the cooked meat of a female mole [85]. Kharpert was an agrarian area, and it was awash with moles that caused great damage to crops. They could also become breeding grounds for certain bacteria (just like mice and rats). These bacteria could spread via moles biting farmers, or farmers coming into contact with moles’ excretions. Diseases spread from one person to another via the puss that oozed from burst blisters. Aside from these general observations, we were unable to find more precise information on the origins and symptoms of khlrtoug.

Various other conditions
- Ouretsvoril (“to be distended”): We have learned that the people of Tadem suffered from conditions caused by the build-up of albumin in their bodies, resulting in swelling. They would treat the condition within a few hours by bathing in an infusion of morning glories (Concolvulus assyricus) in water. This plant grew in the area’s mountains [86]. Albumin is a protein present in blood, which must not find it ways into urine. Otherwise, the patient suffers from a condition called albuminuria, which is a symptom of kidney disease, and would cause swelling in the body. Other herbs used to treat this condition were astragalus, angelica, and rhubarb (rheum) [87].
- Spleen Conditions: This small organ is located above the stomach, on the left side of the abdomen. It purifies the blood, ensures the balance of fluids in the body, and strengthens immunity. The spleen is part of the human body’s lymphatic system. In Tadem, those who suffered from afflictions of the spleen would lose all appetite, lose weight, and “their abdomens would swell like drums.” The old ladies who served as the healers of Tadem would have the patient disrobe and stand in the middle of a frigid stream, then they would use a large knife to trace the shape of a cross three times in the water. They would then proceed to repeat this act on the patient’s abdomen, without, however, seriously injuring the skin. While performing this ritual, they would also chant incantations. If the patient’s condition did not improve within a week, the abdomen would be rubbed with honey [88].
There could be rational explanations for these treatments. Cold water energizes a dormant lymphatic system. The knife play was probably meant to make an impression on the patients. Massaging the abdomen (with or without honey) would undoubtedly invigorate the lymphatic system, helping drain away collected fluids and reducing swelling [89].

Conclusion
It seems strange that the many voluminous, illustrated tomes on the history of Kharpert District contain only isolated bits of information on the folk medicine practiced in the area, while they delve into great details regarding other aspects of local life.
Within this vast district, two cities had become centers of education – Kharpert and Mezire. However, the relatively high level of education found in these locales seems to have had difficulty penetrating the countless agrarian villages dotting the district’s golden valley.
The presence of certain diseases and conditions in Kharpert can be explained by the relatively advanced level of local industry, the use of open-air toilets at inappropriate locations, and the general absence of a sewer system.
The health care guidelines created by Boghos Efendi Dzeron for the Village of Parchandj were perhaps disseminated to neighboring areas, thus benefiting the district’s population. Missionaries also established clinics that improved the level of care received by locals.
Like their compatriots living in other Armenian-populated provinces of the Ottoman Empire, the people of Kharpert utilized a great many superstitious treatments, and firmly believed in miraculous healing. Such beliefs were commonplace at the time, and perhaps continue to be so in all four corners of the world. But in addition to those beliefs and rituals, the people’s innate common sense, the trial-and-error process, and their rational, empirical observations also gave birth to certain objective methods of treatment, such as osteopathy, the use of mineral waters, and the use of herbs and animal matter to treat medical conditions. Many of these treatments were thinly veiled as religious-mystical interventions, and this mysticism manifested itself in the use of sacred numbers (three and seven), incantations, and the belief in punishments resulting from the violations of societal proscriptions or taboos.
As we have seen, the midwives of Kharpert were using primitive intrauterine devices (IUDs), which were very advanced for the time. The conception and ingredients of these medical interventions are exemplary even when judged by modern standards. The importance that the people of Kharpert ascribed to the treatment of infertility is symbolic. Their desire to procreate was likely tied to their urge not to die off in the face of the challenges posed by their environmental physical or political challenges.

Acknowledgements
I thank the Houshamadyan team, which provided me with the primary sources I needed for this article. I also thank Sosse Tertsagian, one the librarians of the Montreal Hamazkayin Library, who recalled several treatments of medical conditions used in Kharpert, and which she had learned from her forebears. I thank Maritz Boudjikanian, who sent me a copy Vahé Haig’s Kharpert yev Anor Vosgeghen Tashde, weighing five kilograms, from Paris. I also thank Ani Boudjikanian for the compact disc (CD) she provided me, containing copies of several books relating to the article’s subject. The CD was prepared in 2017 by the Kharpert Compatriotic Union of Beirut (founded in 1923).
[1] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde [Kharpert and Its Golden Valley], New York, 1959.
[2] Armen Boudjikanian, “Anor Roumpe ir Klkhoun Mech E” [“His/Her Bomb is in His/Her Own Head”], Badmoutyun Boudjikanian Kertasdani [History of the Boudjikanian Clan], Donigian Press, Beirut, 1974, page 6.
[3] Bedros Depoyan, “Kharpert yev Anor Anmichagan Shrchanage” [Kharpert and its Immediate Environs]; Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, New York, 1959, page 27.
[4] “Elazig”, Wikipedia.
[5] Maps of Armenian villages – Harput, “Pinterest.”
[6] Depoyan, page 28.
[7] Manoug K. Djizmedjian, Kharpert yev ir Zavagnere [Kharpert and its Children], Fresno, 1955.
[8] Dindjian, page 37.
[9] Sdepan Dindjian, “Kharpert Kaghakin Taghere” [“The Neighborhoods of the City of Kharpert”], Kharpert yev Anor Vosgeghen Tashde, page 488.
[10] Dindjian, page 638.
[11] Penyamin Nourigian, “Husenig”, Kharpert yev Anor Vosgeghen Tashde, page 739.
[12] Depoyan, page 39.
[13] Manoug B. Dzeron, Parchandj Kugh. Hamaynabadoum (1600-1937) [Parchandj Village. An Encyclopedia (1600-1937)], Boston, 1938, pages 228-229.
[14] Dindjian, pages 661-674.
[15] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, pages 641-643.
[16] Ibid., pages 649-652.
[17] Ibid., pages 656-659.
[18] Ibid., pages 644-648.
[19] Dindjian, page 666.
[20] “Occupational Diseases”, Wikipedia.
[21] Dzeron, Parchandj Kugh, page 130.
[22] Ibid., page 126.
[23] Ibid., pages 130-131.
[24] Ibid., page 119.
[25] Hagop Gharib Shahbazian, Tankaran Kughe. Mer yev Siro Arunod Adzouner [The Village of Tankaran. The Blood-Soaked Nation of our Love], France, 1967, page 63.
[26] Ibid., pages 61-63.
[27] “Semmelweis Ignaz”, Wikipedia.
[28] Dzeron, Parchandj Kugh, page 118.
[29] Adom Boudjikanian, Kayseri – Folk Medicine (<link arm mapottomanempire vilayetankara kayserisandjak localcharacteristics kayserifolkmedicine.html>www.houshamadyan.org/arm/mapottomanempire/vilayetankara/kayserisandjak/localcharacteristics/kayserifolkmedicine.html).
[30] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, page 902.
[31] Daniele Ryman, Elemi – Canarium luzonicum.
[32] Djizmedjian, Kharpert yev ir Zavagnere, page 62.
[33] Ibid., pages 62-63.
[34] Ibid., page 63.
[35] G. H. Aharonian (editor), Huseinig, Hairenik Printing Press, Boston, 1965, pages 133-138.
[36] Ibid., pages 134-136.
[37] Ibid.
[38] Ibid., pages 134-138.
[39] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, page 885.
[40] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, page 898.
[41] Susie Hoogasian Villa/Mary Kilbourne Villa, Armenian Village Life Before 1914, Wayne State University Press, 1982, pages 96-67.
[42] “Female Infertility, Symptoms and Causes”, Mayo Clinic.
[43] Andrew Chevallier, “Clou de Girofle”, in Encyclopedie des plantes médicinales, page 97.
[44] Hamel Chaieb et al., “Clove oil, Eugenia caryophyllata”, Phytotherapy Research, Volume 21, Issue 6, March 2007.
[45] Ibid.; “Gingembre”, page 155.
[46] Ghayur MN et al., “Inhibitory activity of ginger rhizome on airway and uterine smooth muscles preparations.”
[47] Al-Snafi Ali Esmail, “The medical importance of Cicer arietinum, a review”, IOSR Journal of Pharmacy, Volume 6, Issue 3, March 2016, pages 29-40.
[48] Hoogasian Villa/Kilbourne Villa, Armenian Village Life, page 98.
[49] Ibid., page 112.
[50] Natural Medicines, comprehensive database.
[51] Hoogasian Villa/Kilbourne Villa, Armenian Village Life, pages 112-113.
[52] “Breastfeeding during pregnancy: safety and challenges”.
[53] Tertsagian, interview, May 2018.
[54] Shahbazian, Tankaran Kughe…, page 58.
[55] Merck Manual, Whyley, 2009, pages 1217-1218.
[56] McCall W. Wade, “Chicken Manure”, Hawaii Cooperative Extension Service, College of Tropical Agriculture, 1980.
[57] Schenkels Leon CP M. et al, Abstract, «Biochemical composition of human saliva...”, Department of Oral Biochemistry, Vrije University, Amsterdam.
[58] Habousi Kughin Badmoutyune [The History of the Habous Village], Baykar Press, Boston, 1963, page 72.
[59] Ibid.
[60] Tertsagian, interview, May 2018.
[61] Shahbazian, Tankaran Kughe…, pages 58-59.
[62] Singh CP et al., “Characterization of antiviral and antibacterial Bombix mori seroin proteins”, April 2, 2014.
[63] Shahbazian, Tankaran Kughe, pages 53-54.
[64] Untitled Booklet on Mercurochrome in First Aid, booklet not dated.
[65] Djizmedjian, Kharpert yev Ir Zavagnere, page 400.
[66] Thompson T., “Is alcohol effective as a pain killer?”, www.bodymind.org/alcohol
[67] Shahbazian, Tankaran Kughe, page 56.
[68] Ibid., page 54.
[69] Ibid., pages 60-61.
[70] Djizmedjian, Kharpert yev Ir Zavagnere, page 400.
[71] Ibid., pages 398-399.
[72] Kevorkian/Paboudjian, Les Arméniens dans l’Empire Ottoman à la Veille du Génocide, 1992, Paris, pages 365-366.
[73] Djizmedjian, Kharpert yev Ir Zavagnere, page 400.
[74] Ibid.
[75] Mayo Clinic, Scarlet Fever.
[76] Vahé Haig, Kharpert yev Anor Vosgeghen Tashde, page 929.
[77] Antimicrobial plants, Google search.
[78] Shahbazian, Tankaran Kughe…, page 56.
[79] Merck Manual, Malaria, pages 1218-1220.
[80] Shahbazian, Tankaran Kughe…, page 55.
[81] Adult Jaundice, Cleveland Clinic. www.clevelandclinic.org.
[82] Baron S. et al., Abstract, “Antiviral activity in urine is attributable to ammonium salts”, 1989, J. Biol Regul Homeost Agents.
[83] Tertsagian, interview, May 2018.
[84] Shahbazian, Tankaran Kughe…, pages 59-60.
[85] Ibid., page 61.
[86] Ibid., page 57.
[87] Peng et al., “Herbal treatment for renal diseases, a review article”, Abstract, Annals of Academic Medicine, Singapore, January 2005, Vol 34, N. 1, pages 44-45.
[88] Shahbazian, Tankaran Kughe, pages 57-58.
[89] Edele C.F., “Manual lymph drainage for equine lymphoedema – treatment strategy and therapist training.”